When a joint pain or joint tenderness exhibits, it might be solely mistaken for arthritis –a common condition that causes pain and inflammation in the joints. In fact, if swollen or tender joints are present with scaly skin patches, psoriatic arthritis might be indicated. If it is left untreated, some patients with psoriatic arthritis can further develop a severe and disabling form of arthritis. Over time, arthritis destroys the small bones, leading to permanent deformity and disability.
Get to know psoriatic arthritis
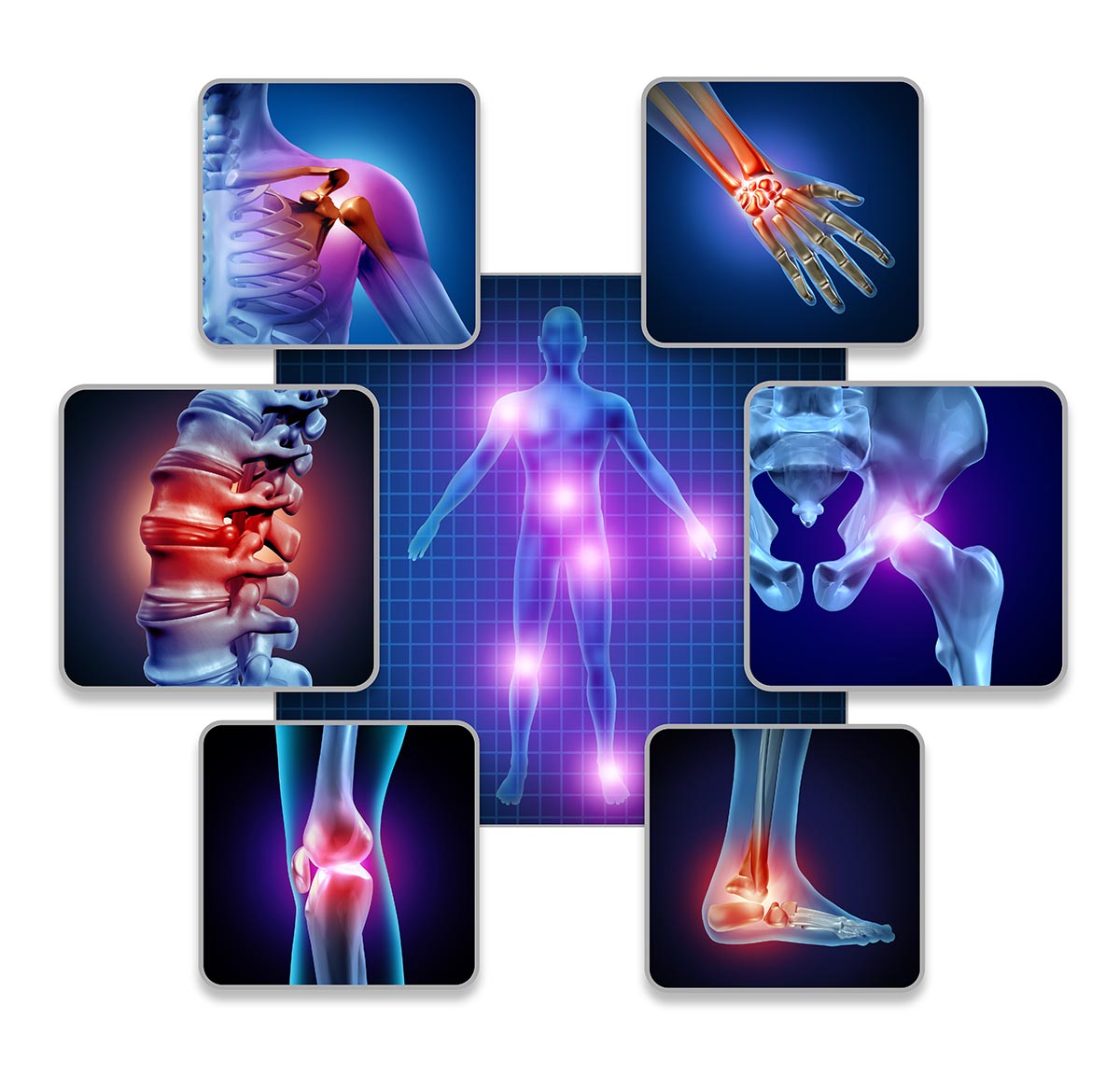
Psoriasis is an immune system condition that causes the skin to inflame and regenerate at faster rates. This rapid turnover of skin cells results in scales and red patches. Psoriasis patches can widely range from tiny spots of scaling to major eruptions that cover large areas of the body, such as lower back, elbows, knees, legs, soles of the feet, scalp, face and palms. There are approximately 35% of the patients with psoriasis have arthritis with joint and back pain. This condition is known as psoriatic arthritis. The most common signs and symptoms of arthritis involve the joint pain, stiffness, swelling and redness. Pain or tenderness can manifest in different forms, affecting either one or multiple joints. Chronic arthritis can induce high degree of inflammation, resulting in swollen fingers. In some cases, migratory arthritis occurs when pain spreads from one joint to another. The first joint may start to feel better before pain starts in a different joint. Some forms of arthritis can cause back pain, leading to loss of flexibility in the spine. In addition, some patients might experience foot pain, especially in the sole or the Achilles tendon.
In patients who have spinal arthritis, back pain and back tenderness are major symptoms. Pain often worsens after getting up in the morning (morning stiffness) or holding still for a while. The stiffness usually loosens and goes away after movement. However, it can take some time. In some cases, pain might appear in the lower back or below the waist.
Diagnosis
Apart from medical history taking and a comprehensive physical examination, diagnostic tests involve:
- Blood test. Blood test aims to determine levels of certain substances in the blood that strongly indicate inflammation.
- X-rays. Plain X-rays can help pinpoint changes in the affected joints.
- Ultrasound uses high-frequency sound waves to visualize the inflammation of soft tissues, cartilage and fluid-containing structures near the joints (called bursae).
- Magnetic resonance imaging (MRI) with contrast media. MRI with contrast media combines radio waves with a strong magnetic field, allowing for more-detailed cross-sectional images of soft tissues, such as cartilage, tendons and ligaments. This imaging test is often used to identify the inflammation in spinal ligaments or joints that connect sacrum to the hip bone (sacroiliac joints).
In patients manifested only with back pain or pain in the waist area, MRI scan of the spine is essentially required in order to role out other spinal diseases and conditions, e.g. disc herniation and ankylosing spondylitis. However, if pain presents in the lower back, MRI scan of lumbar spine and sacrum should be performed for a full investigation.
Treatment
Treatment goal of psoriatic arthritis aims at controlling inflammation in affected joints in order to delay disease progression and prevent disability. Several treatment options are available, depending on individual’s conditions and disease severity.
- Monoarthritis: For single joint inflammation, primary treatment involves steroid injections into an affected joint to reduce inflammation. After steroid administration, treatment follow-ups are required.
- Polyarthritis: If more than one joint is affected, treatment plan is primarily made based upon laboratory and imaging results. In non-severe cases, disease-modifying antirheumatic drugs (DMARDs) are often prescribed, such as methotrexate and sulfasalazine. If arthritis severely progresses, a newer class of DMARDs known as biologic agents (biologic response modifiers) can be administered for a quicker response to mitigate the inflammation. These medications selectively target specific parts of the immune system that trigger inflammation and lead to joint damages.
- Back pain and stiffness: Initial treatment typically includes nonsteroidal anti-inflammatory drugs (NSAIDs) that can relieve pain and inflammation. If disease severity does not subside with intensifying symptoms, instead of using conventional disease-modifying antirheumatic drugs (DMARDs), treatment is principally shifted to biologic response modifiers for an improved clinical outcome. Although a number of novel drugs used to treat arthritis and psoriatic arthritis have been emerged, drug selection and treatment regimen will be determined in accordance with disease severity and skin conditions as well as medical history and previous treatments of individual.
If psoriatic arthritis cannot be treated in a timely manner, besides severe skin inflammation, it can potentially lead to joint deformity or even long-term disability. Psoriatic arthritis can be discouraging since the pain is compounded by limited ability to continue daily lives and tasks. If warning sign and symptom indicates, immediate medical attention should be sought, enabling an accurate diagnosis and effective treatment before the condition progresses along with other serious complications.









