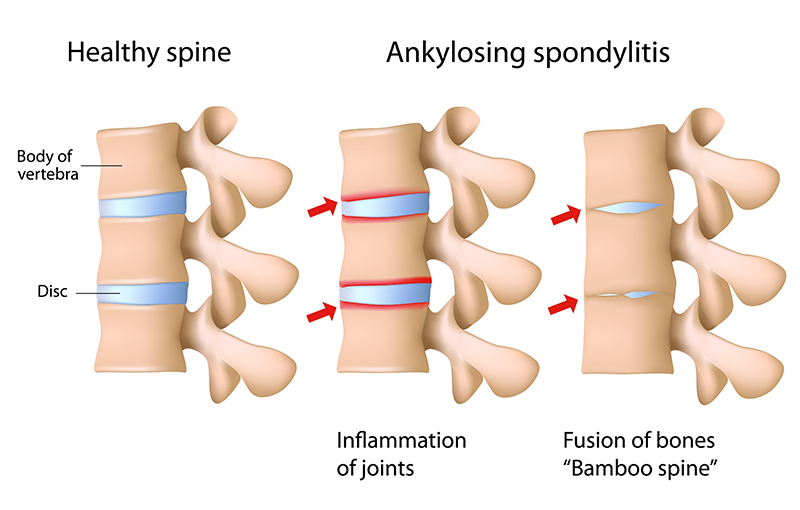
Back pain with different severity degrees can be caused by a wide range of medical conditions. Acute back pain can be treated effectively if accurate diagnosis can be timely made. However, if back pain progresses to chronic and severe pain without adequate response to given treatments, it might strongly indicate arthritic disease, called ankylosing spondylitis. Ankylosing spondylitis is defined as an inflammatory disease that, over time, can cause some of the small bones in the spine (vertebrae) to fuse. This fusing makes the spine less flexible, resulting in stiffness and chronic back pain that can largely interfere with quality of life. If warning signs and symptoms of ankylosing spondylitis arise, medical attention and treatment must be sought immediately.
Get to know ankylosing spondylitis
Spondyloarthritis is a group of diseases characterized by inflammation in the spine (spondylitis) and joints (arthritis). Ankylosing spondylitis is one type of spondyloarthritis, defined as a long-term inflammation of the joints of the spine. In severe cases, the body attempts to heal by forming new bones with calcium deposits which gradually fuse sections of vertebrae. This fusion can stiffen the spine, leading to less flexibility, severe back pain and inability to move. In some patients, stiffness of other joints might be present e.g. ankle, knee and hip. Other manifestations of other organs that are induced by chronic inflammation besides spine and joints often include red eyes, blurred vision, pain in the heel or arch of the foot and psoriasis –an autoimmune disease that manifests in the form of scaly red and silvery skin patches.
Causes and risk factors
Definite cause of ankylosing spondylitis remains unknown, although genetic alterations seem to be involved. People who have the HLA-B27 gene are at a greatly increased risk of developing ankylosing spondylitis. However, other contributing factors are certain infections and exposure to particular substances. Men are more likely to develop ankylosing spondylitis than are women while onset generally occurs in late adolescence or early adulthood.
Signs and symptoms
Symptoms of ankylosing spondylitis include:
- Chronic pain or stiffness in the back lasting longer than 3 months without traumatic injuries, overuse or repetitive movement of the back muscles.
- Stiffness or pain in the back during night time, while sleeping and after waking up in the morning.
- Stiffness or pain in the back after periods of inactivity.
- Joint pain and inflammation in the lower part of the body, such as hip, knee and ankle.
Other manifestations e.g. fatigue, red eyes and eye pain, mouth ulcer, skin rash and loss of appetite.
Diagnosis
Diagnostic tests of ankylosing spondylitis usually involve:
- Medical history: The doctor conducts medical reviews to identify pain location, pain intensity and duration as well as to collect patient’s medical history.
- Physical examination: During physical examination, the doctor might ask the patient to bend in different directions for testing the range of motion in the spine. The doctor reproduces the pain by pressing on specific portions of the pelvis or by moving the legs into particular positions.
- Blood tests: Blood tests can check for markers of inflammation and the HLA-B27 gene which is a major factor to develop the disease. Nonetheless, people who have this gene might not have ankylosing spondylitis and vice versa, patient can develop the disease without having this gene.
- X-ray: X-ray is an imaging test to identify the location of inflammation and fusion as well as wear and tear of the spine.
- MRI scan: An MRI uses radio waves and a strong magnetic field to provide more-detailed images of bones and soft tissues. With high degree of accuracy, MRI scans can reveal evidence of early disease and help to plan treatment as well as monitor treatment outcomes during follow-ups.
Treatments
Based primarily on current treatments, there is no cure for ankylosing spondylitis. However, treatments can alleviate symptoms, reduce inflammation and possibly prevent complications as well as slow progression of the disease, resulting in minimized risks of long-term disability. Treatment options include:
- Medications: To relieve pain and stiffness, common medicines prescribed in patients with ankylosing spondylitis are pain killer drugs, nonsteroidal anti-inflammatory drugs (NSAIDs) and anti- rheumatic drugs as well as other groups of medications. Since some of these medicines may produce side effects or adverse drug reactions, they must be taken strictly as instructed by the pharmacists.
- Physical therapy: Physical therapy provides a number of benefits, from pain alleviation to improved physical strength and preserved good posture. A wide variety of treatment to relieve pain include stretching, massage, exercising, joint mobilization or manipulation, cryotherapy and ultrasound.
- Surgery: Surgery might be recommended if patients have severe pain or joint damage and poor posture caused by joint stiffness. Surgery helps to restore range of motion of the spine and improve quality of life.
- Lifestyle changes: Lifestyle modification that can help improve the symptoms include avoid using a pillow that is too high or too stiff, avoid bending positions, practice good posture and lie flat with straight back
- Other treatments: If complications develop, treatments given by the specialists are further needed, such as eye inflammation (uveitis) and heart problems.
Chronic back pain should not be overlooked since it might indicate ankylosing spondylitis. If left untreated, spine eventually becomes inflexible and fusion can stiffen the rib cage as well as restrict heart and lung functions, resulting in serious complications and long-term disability. Accurate diagnosis and effective treatments must be timely applied in order to relieve back pain, slow disease progression and prevent other complications that may arise.