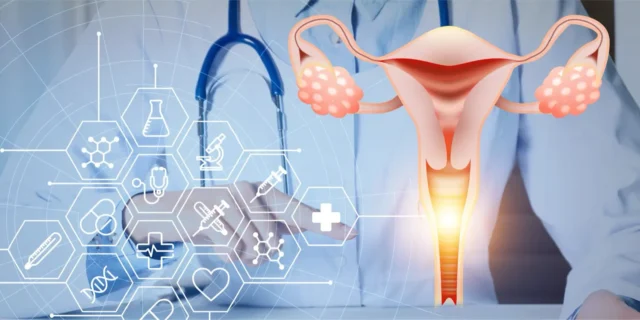
Gynecologic oncology is a subspecialty of obstetrics and gynecology that focuses on the prevention, diagnosis, treatment, and management of malignancies of the female reproductive tract. It integrates surgical, chemotherapeutic, and radiation-based interventions, often in multidisciplinary settings.
Major Types of Gynecologic Cancers
Gynecologic oncologists typically treat the following cancers:
- Cervical Cancer
- Originates in the cervix, the lower part of the uterus.
- Often caused by persistent infection with high-risk human papillomavirus (HPV).
- Detected via Pap smears and HPV testing.
- Ovarian Cancer
- Starts in the ovaries but can also include fallopian tube and primary peritoneal cancers.
- Often diagnosed at a late stage due to vague symptoms.
- Includes epithelial, germ cell, and stromal tumors.
- Endometrial (Uterine) Cancer
- Arises from the lining of the uterus (endometrium).
- Most common gynecologic cancer in developed countries.
- Linked to unopposed estrogen exposure and obesity.
- Vulvar Cancer
- Affects the external genitalia.
- Often associated with HPV or lichen sclerosus.
- Presents as a lump, ulcer, or chronic itching.
- Vaginal Cancer
- Rare cancer that occurs in the vaginal canal.
- Often secondary (spread from cervix or vulva).
- Usually squamous cell carcinoma.
- Gestational Trophoblastic Disease (GTD)
- A group of rare tumors involving abnormal growth of cells inside a woman’s uterus.
- Includes hydatidiform mole and choriocarcinoma.
Signs and Symptoms of Gynecologic Cancers
Gynecologic cancers affect the female reproductive organs and often present with vague or nonspecific symptoms, especially in early stages. Awareness of these symptoms can lead to earlier diagnosis and better outcomes.
1. Cervical Cancer
Often asymptomatic in early stages due to slow progression from precancerous lesions.
Common Symptoms:
- Abnormal vaginal bleeding, especially:
- After intercourse (postcoital bleeding)
- Between periods
- After menopause
- Unusual vaginal discharge (watery, foul-smelling, or bloody)
- Pelvic pain or pain during intercourse (dyspareunia)
Note: Routine Pap tests and HPV screening are essential for early detection.
2. Ovarian Cancer
Often called the “silent killer” because symptoms are nonspecific and often misattributed to gastrointestinal or urinary issues.
Early Symptoms (subtle but persistent):
- Bloating
- Pelvic or abdominal pain
- Difficulty eating or feeling full quickly
- Frequent or urgent urination
Other Possible Symptoms:
- Fatigue
- Indigestion
- Back pain
- Menstrual irregularities
- Pain during intercourse
Note: Persistence (>12 days per month) or worsening of these symptoms is key.
3. Endometrial (Uterine) Cancer
Most common gynecologic cancer in high-income countries. Often diagnosed early due to noticeable symptoms.
Primary Symptom:
- Abnormal uterine bleeding, including:
- Postmenopausal bleeding (most common red flag)
- Bleeding between periods
- Heavy or prolonged periods
Other Symptoms:
- Pelvic pain or pressure
- Unusual vaginal discharge (especially in postmenopausal women)
4. Vulvar Cancer
Often diagnosed in older women but increasingly seen in younger women due to HPV.
Common Symptoms:
- Itching, burning, or soreness in the vulvar area
- Lump, ulcer, or wart-like growth
- Bleeding or pain not related to menstruation
- Changes in skin color or texture
Note: Persistent vulvar irritation or lesions should be biopsied.
5. Vaginal Cancer
A rare cancer, often secondary to spread from cervix or vulva.
Possible Symptoms:
- Abnormal vaginal bleeding, especially after intercourse
- Watery or bloody vaginal discharge
- Pelvic pain
- Mass or sensation of fullness in the vagina
- Pain during urination or bowel movements
6. Gestational Trophoblastic Disease (GTD)
A group of rare tumors that develop from abnormal pregnancy tissue.
Symptoms:
- Abnormal uterine bleeding during or after pregnancy
- Enlarged uterus not consistent with gestational age
- Severe nausea and vomiting (hyperemesis gravidarum)
- Passage of grape-like cysts (in molar pregnancy)
- Very high β-hCG levels
General Red Flags for Gynecologic Cancer
Seek medical evaluation if you have:
- Postmenopausal bleeding
- Bleeding after sex
- Persistent bloating or abdominal swelling
- Chronic pelvic or back pain
- Unexplained weight loss or fatigue
- Unusual vaginal discharge
- Any vulvar or vaginal lesion that doesn’t heal
Diagnosis
- Pelvic examination
- Pap-smear (for cervical cancer)
- Imaging: Ultrasound, CT, MRI, PET scans
- Biopsy: Tissue sampling for histopathology
- Blood Tests/ Tumor markers: CA-125 (ovarian), hCG (GTD)
Prevention and Screening
- HPV vaccination: Reduces risk of cervical and other HPV-associated cancers
- Pap smear and HPV co-testing: Screening for cervical cancer regularly
- Genetic counseling and testing: BRCA mutations (ovarian, breast), Lynch syndrome (endometrial)
- Knowing your family history of cancer
- Maintaining a healthy weight and lifestyle
Treatment Modalities
Treatment depends on cancer type, stage, and patient factors, and may include:
- Surgery: Hysterectomy, oophorectomy, lymph node dissection, Cytoreductive (debulking)
- Radiation therapy: External beam or brachytherapy
- Chemotherapy: Often platinum-based for ovarian cancer
- Targeted therapy: PARP inhibitors, angiogenesis inhibitors
- Immunotherapy: Especially in cervical cancer (e.g., PD-1 inhibitors)
Follow-Up and Surveillance
Surveillance Strategies (variable by cancer type and stage):
- Every 3–6 months for 2 years, then every 6–12 months for 3–5 years.
- History and physical exam, including pelvic exam.
- Imaging and tumor markers as indicated (e.g., CA-125).
- No role for routine cytologic screening post-hysterectomy for non-cervical cancers.