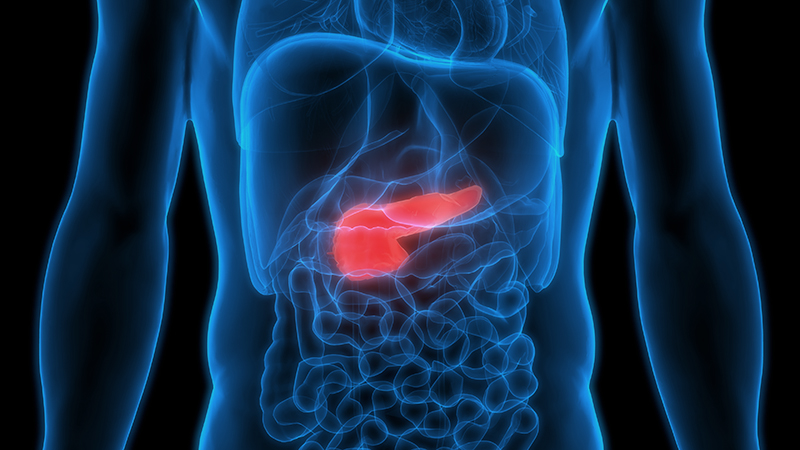
The pancreas is an organ located in the abdomen and is a part of the digestive system of the body. It plays a crucial role in converting the food we consume into energy for the body. The pancreas produces essential enzymes required for digestion and certain hormones that regulate blood sugar level (glucose). Although signs and symptoms of pancreatic diseases might widely vary among individuals, depending on disease severity, patients with pancreatic diseases might experience no warning symptom until their conditions progress to advanced stages which become more difficult to be completely cured. Being aware of warning signs remains important, allowing for an early diagnosis and effective treatment in a timely manner.
Get to know the pancreas
The pancreas is an organ that people are often confused with the liver despite the fact that these two organs are located in different locations in the abdomen. However, liver and pancreatic diseases often share similar manifestations, leading to inaccurate or delayed diagnosis. The pancreas is a long, flat gland positioned behind the stomach in the upper abdomen. The head of the pancreas is on the right side of the abdomen and it is connected to the first section of the small intestine, called the duodenum. Whereas the tail which is the narrow end extends to the left side of the body. The pancreas is surrounded by other important organs in the abdomen, including the spleen, liver and small intestine.
The roles of the pancreas
The pancreas plays a vital role in converting the food into energy that the body requires. It mainly performs two functions:
- An exocrine function: The pancreas produces several enzymes that help digestion of carbohydrates, lipids and proteins. Essential enzymes produced by the pancreas are, for example, amylase and lipase.
- An endocrine function: The pancreas also creates and releases certain hormones that regulate blood sugar levels, e.g. insulin (acting to lower blood sugar) and glucagon (acting to raise blood sugar). Therefore, pancreatic abnormalities substantially affect digestive functions and impair blood sugar control.
Pancreatic diseases
Similar to other organs, there is a wide range of pancreatic conditions triggered by different factors. Among these, pancreatitis and pancreatic cancer are frequently diagnosed.
- Acute pancreatitis
Pancreatitis is a disease in which the pancreas becomes inflamed when the digestive enzymes are activated before they are released into the small intestine and these enzymes begin to attack the pancreas, causing inflammation. Acute pancreatitis appears suddenly and normally lasts for days. Signs and symptoms of acute pancreatitis may vary, extending from mild to life-threatening. Manifestations in each individual hinge upon disease severity.
Causes of acute pancreatitis: Two major causes that potentially contribute to acute pancreatitis are excessive alcohol consumption and gallstones. Researches have demonstrated that heavy alcohol users are at greater risk of pancreatitis. However, the chance of developing pancreatitis is principally determined by the amount and duration of alcohol drinking. Gallstones are frequently considered another risk factor of pancreatitis. Patients with gallstone-induced acute pancreatitis might not experience any warning sign of gallstones until acute pancreatitis arises.
Signs and symptoms: Acute pancreatitis exhibits signs and symptoms, including:
- Severe and sudden abdominal pain in the upper abdomen under the right ribs.
- Abdominal pain that might radiate to the back.
- Low-grade or high-grade fever when the condition progresses.
- Jaundice presented with yellow discoloration of the skin and whites of the eyes.
Severity of acute pancreatitis: Signs and symptoms are varied among individuals, depending on the degree of inflammation. In patients with mild pancreatitis, abdominal pain is usually tolerable and resolved spontaneously within 1-3 days. Whereas in some patients whose conditions progressively advance and develop severe pancreatitis, they might exhibit severe and intense abdominal pain which further triggers systemic inflammatory response induced by pro-inflammatory cytokines. If it is left untreated, it can possibly result in fatal complications such as necrotizing pancreatitis – a condition where parts of the pancreas die due to lack of sufficient blood supply.
- Chronic pancreatitis
With repeated bouts of acute pancreatitis, damages to the pancreas can lead to chronic pancreatitis. Over time, structural alteration, scar tissue and calcification may form in the pancreas, causing loss of its function. In addition, gallstone pancreatitis might be concurrently discovered.
Causes of chronic pancreatitis: Chronic pancreatitis is caused mainly due to long-term alcohol consumption. Nevertheless, chronic pancreatitis can be also found in non alcohol drinkers. Besides overuse of alcohol, hereditary chronic pancreatitis – a rare genetic disorder predisposes a person to develop the disease.
Signs and symptoms of chronic pancreatitis: Without appropriate treatments, chronic pancreatitis can lead to life-threatening complications. Predominant symptom is chronic abdominal pain in the upper abdomen which sometimes suddenly occurs. With repeated episodes, chronic pancreatitis significantly impairs patients’ quality of life. Severe abdominal pain, unintentional weight loss and loss of work are the significant factors most closely associated with poor health status perception.
Severity of chronic pancreatitis: Complications caused by chronic pancreatitis often include:
- Poorly functioning pancreas, causing digestion problems and diabetes.
- Fibrosis and scarring due to progressive pancreatic inflammation, leading to common bile duct compression and jaundice.
- Scarring, leading to small intestine obstruction or blockage which largely interrupts with eating ability.
- Increased risk of developing pancreatic cancer
- Cancer of the head of the pancreas
The head of the pancreas is on the right side of the abdomen, behind where the stomach meets the first part of the small intestine. Pancreatic cancer arises when cells in the pancreas begin to multiply out of control and form a mass. Pancreatic cancer appears differently, depending on which part of the pancreas the tumor is formed, whether the head or the tail. In fact, pancreatic cancer often occurs in the head of the pancreas. Although the definite cause remains unknown, smoking, chronic pancreatitis and intraductal papillary mucinous neoplasm (IPMN) – a tumor that can occur within the cells of the pancreatic duct significantly increase the risk of pancreatic cancer.
Diagnosis: Owning to the absence of any warning sign and symptom, pancreatic cancer appears to be difficult to diagnose early. Currently, there is no standard diagnostic approach or established method to early detect pancreatic cancer yet. Blood tests or imaging results usually cannot be used to early detect this disease. Early stage of pancreatic cancer is usually detected if the location of the pancreatic cancer causes presenting symptoms early. Patients often seek medical attention when their conditions progress to advanced stages.
Signs and symptoms: The most common signs and symptoms that urge the patients to get medical assistance include:
- Jaundice caused by the obstruction of bile ducts
- Dark-colored urine
- New diagnosis of diabetes or existing diabetes becomes more difficult to control
Severity: If cancerous mass enlarges or condition progresses, it might lead to:
- Small intestine obstruction: Pancreatic cancer that grows into or presses on the first part of the small intestine can block the flow of digested food from the stomach into the intestines, leading to loss of appetite and rapid weight loss.
- Severe abdominal pain in the upper abdomen under the right ribs: A growing pancreatic tumor may press on nerves in the abdomen, causing pain that can become severe.
- Ascites: If pancreatic cancer has spread into the abdomen, extra fluid buildup in the abdomen or ascites might develop, causing the stomach to swell and stretch out.
- Cancer of the tail of the pancreas
The tail of the pancreas is located on the left side of the abdomen. Since this part is not adjacent to the common bile ducts, pancreatic cancer at the tail is more likely to result in abdominal pain in the upper left abdomen, under the left ribs without the presence of jaundice.
Diagnosis of pancreatic diseases
The evaluation of pancreatic diseases can be quite challenging due to the inaccessibility of the pancreas. To make an accurate diagnosis leading to effective treatments, well-trained and highly experienced specialist is crucially needed. There are multiple methods used to evaluate the pancreas, including a medical history taking, physical examination, blood tests and other imaging tests. Diagnostic methods frequently used to detect pancreatic abnormalities include:
- Blood test to evaluate pancreatic enzymes, e.g. amylase and lipase. When acute pancreatitis develops, these enzymes usually rise rapidly. Nonetheless, other conditions can also alter the levels of these pancreatic enzymes, thus laboratory results must be thoroughly interpreted by the specialist.
- Blood test to evaluate CA19-9 which is a specific protein or tumor marker shed by pancreatic cancer cells. High levels of CA 19-9 are often a sign indicating pancreatic cancer. However, the level of CA19-9 should not be used as a confirmative indicator to make a definite diagnosis of pancreatic cancer since the sensitivity and specificity of CA19-9 in detecting pancreatic cancer are fairly limited, signifying that the rise of CA19-9 can indicate other types of cancer or certain noncancerous disorders. On the contrary, some patients with pancreatic cancer do not have elevated CA19-9 levels, therefore the test is not used by itself to screen for or diagnose pancreatic cancer.
- Imaging tests that create detailed pictures of internal organs. These tests, e.g. computerized tomography (CT) scan of the pancreas (CT) and magnetic resonance imaging (MRI) or magnetic resonance cholangiopancreatography (MRCP) help the specialist visualize any abnormality of the pancreas and surrounding areas in the abdomen. Detailed images obtained from these imaging tests can potentially reveal whether the detected mass is cancerous. If the suspected tumor is likely to be cancerous, metastasis or the spread of cancer cells to new areas of the body must be also assessed.
- Using an endoscopic ultrasound (EUS). An ultrasound device is used to create images of the pancreas from inside abdomen. The device is passed through a thin, flexible tube (endoscope) down an esophagus into the stomach in order to obtain the images. Most often the tissue can be collected during EUS by passing special tools through the endoscope. Pathological assessment is then deployed to firmly diagnose pancreatic cancer and guide for appropriate treatment regimens.
Treatment of pancreatic diseases
Treatments for pancreatic diseases depend on diagnosed conditions and severity. Treatment for pancreatitis usually involves non-surgical approaches. If pancreatic tumor or cancer is suspected, surgery is considered a principal treatment. Type of surgery and additional treatments are determined by the stage and location of the cancer as well as patient’s overall health and personal preferences. Due to the complex structure of the pancreas, pancreatic surgery must be performed by the surgeon specialized in the hepatopancreatobiliary system. Cutting-edge technology and medical advances in surgery contribute to minimally invasive surgical techniques with greater precision and enhanced safety that improve surgical outcomes. For instance, vascular resection and reconstruction can be conducted if pancreatic tumors are exhibited along with vascular compression or invasion. In addition, minimally invasive pancreatic surgeries are increasingly adopted worldwide owning to superior advantages, such as less pain, fewer post-operative complications and faster recovery time.
To lower the risk of developing pancreatic diseases, it is highly recommended to:
- Stop or limit drinking alcohol
- Choose a low-fat diet, e.g. fresh fruits, vegetables and lean proteins.
- Regularly exercise.
- Have an annual check-up regularly.
If any warning sign or symptom arises, do not wait. Immediate medical attention must be sought as soon as possible.