Osteoporosis is a disease that causes bones to become weaken and brittle, such that a bone can break by itself or through only a slight force – for example, a fall while standing or walking.
Causes of Osteoporosis
- Hereditary or naturally with age. As people get older, their sex hormones also decrease, and this causes the bones to lose their density – for example, menopause women.
- Other diseases or certain medications. These include thyrotoxicosis, hyperthyroidism, high cortisol levels, steroids, certain types of aromatase inhibitor, and others.
People Who Are at Risk of Osteoporosis
- Women 65 and older as well as men 70 and above.
- Women with low estrogen level: for example, women who are already in menopause before the age of 45, or had complete oophorectomy, or have other chronic diseases, or have undergone strenuous exercises for extended periods, or are taking aromatase inhibitors medication.
- Men with a disease or medication that reduces testosterone levels: for example, medicine that treats prostate cancer, or Klinefelter’s syndrome, etc.
- A person who takes steroids equivalent to 5 mg of Prednisolone or more, continually for 3 months or more.
- A person whose father or mother has had broken hips from a minor accident.
- An underweight person: i.e., less than 20 kg/sqm.
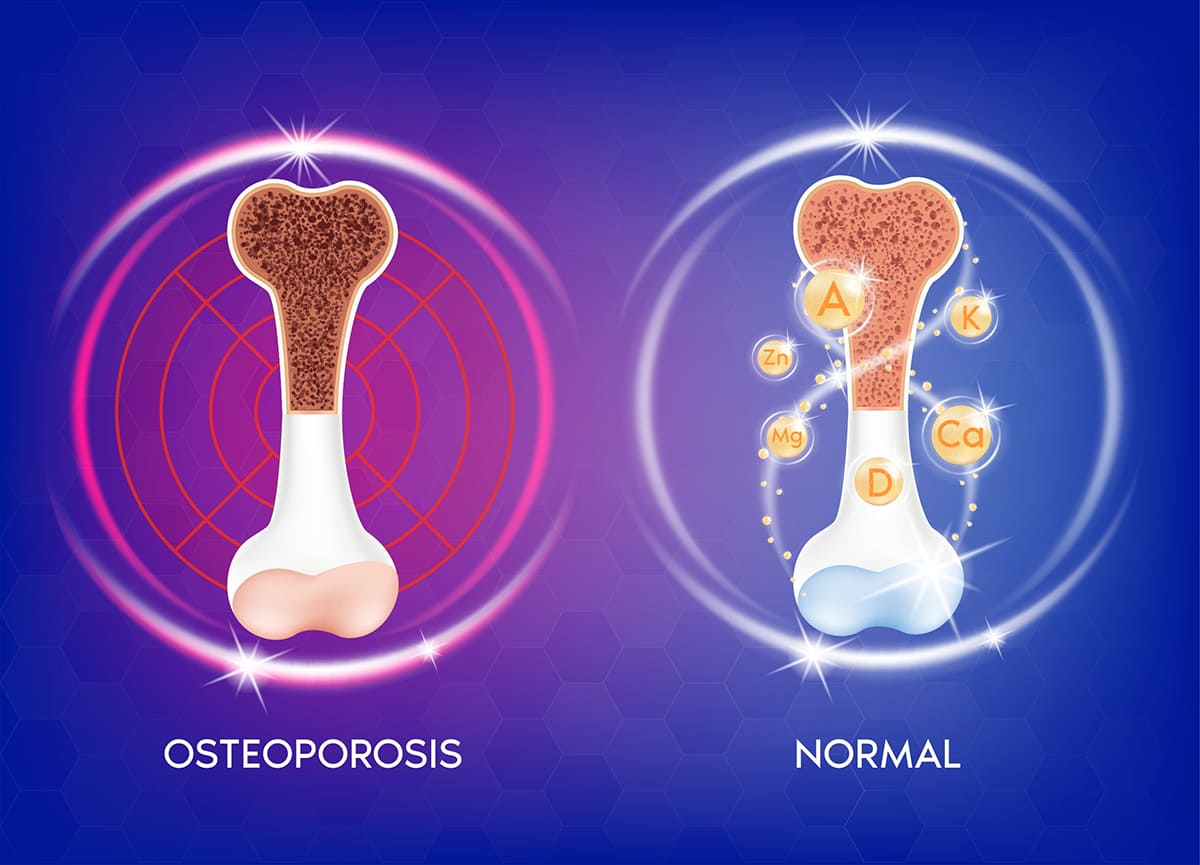
- Other factors, such as people who consume lots of alcohol, smoke, have calcium deficit or low vitamin D in blood stream, and lack exercises.
Symptoms of Osteoporosis
Generally, there is no initial symptom but it will become apparent once a bone is broken. For example, back pain after the spine is broken, reduced height, hunch over. In the case of a broken hip as a result of a fall while standing or walking, the patient will experience severe pain in the hips area as the bone is misaligned; making it difficult for the patient to walk and can become bedridden if without surgery.
Screening for Osteoporosis
This is determined by calculating Osteoporosis Self – Assessment Tool for Asians (OSTA) Score or Khon Kaen Osteoporosis Study (KKOS) Score. Both use patient’s age and weight in the calculation. If the result is less than -1, it means the patient is highly susceptible to osteoporosis. In such a case, the patient should further undergo bone density check.
Osteoporosis Diagnosis
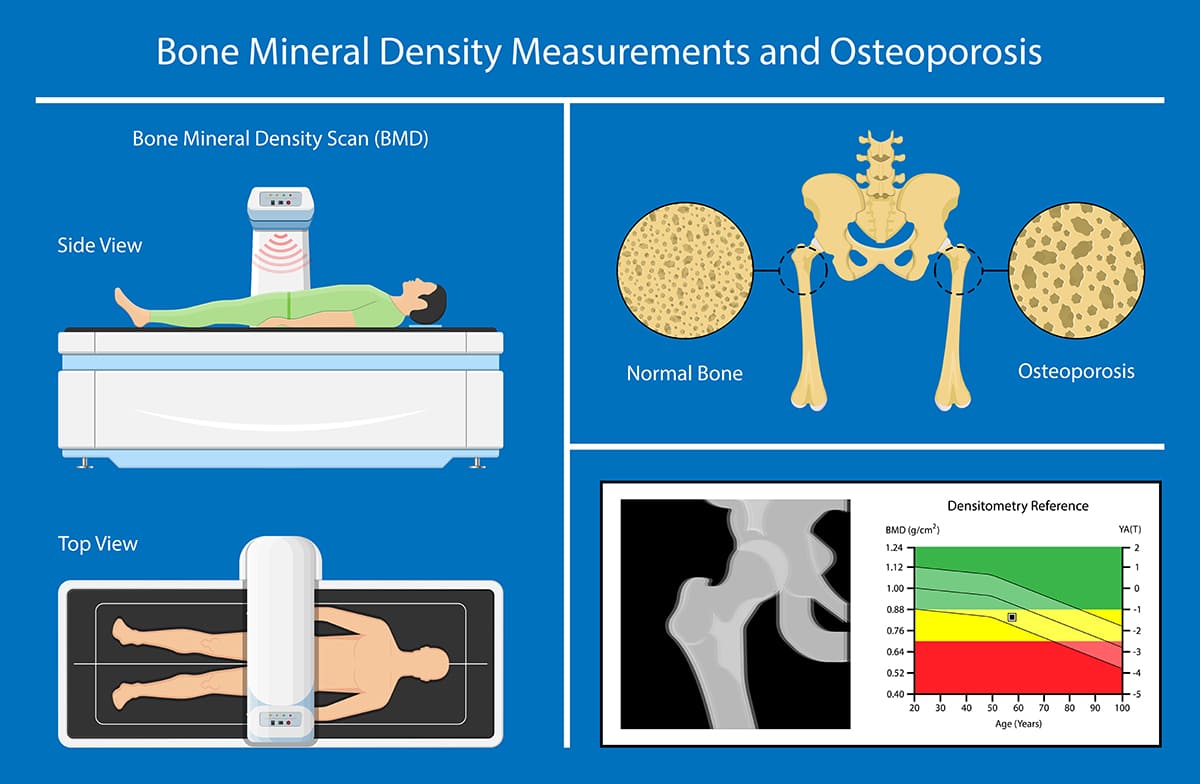
Osteoporosis is diagnosed through bone mineral density (BMD) check using Dual-Energy X-Ray Absorptiometry (DEXA) equipment. Generally, the primary areas for the test are spine and hip bones. If it is not possible to access these locations, the wrist bone (distal radius) is tested instead. The result is the T-Score, by comparing your bone density to the average of the highest values among people of the same gender. A score between -1 and -2.5 suggests osteopenia, while a score of -2.5 or less indicates the presence of osteoporosis.
Osteoporosis Treatment
- Before treating osteoporosis, it is necessary determine its cause. This could be, for example, thyrotoxicosis, hyperthyroidism, escalated level of cortisol, or medication that can cause osteoporosis. If the underlying disease is found, then it must be treated; or if it is medication, then that, too, has to stop.
- Take sufficient amount of calcium. 1,000 – 1,200 mg per day is recommended. This can mainly be from natural food such as milk and dairy products, tofu, small fishes, small shrimps, green vegetables, and sesame. If that proves to be insufficient, then dietary supplements could be added: such as calcium carbonate, which must be taken with or immediately after a meal for best efficacy.
- Receive sufficient dose of vitamin D from food or through dermal synthesis of the sunlight. The recommended amount of vitamin D is around 600 – 800 units per day. In food, it can be found in fish oil, salmon, sardine, tuna, and mushrooms. If additional vitamin D is required, dietary supplements could be considered: for example, ergocalciferol (vitamin D2) or ergocalciferol (vitamin D3). The goal is to maintain more than 30 ng per ml of 25 hydroxy vitamin D in the blood.
- Regular exercises. These should be weight-bearing aerobic activities – such as jogging, brisk walking, dancing – and muscles strengthening as well as balancing exercises. All of these activities will help prevent broken bones.
- Quit smoking and reduce alcohol consumption. Alcoholic beverages should not be more than 3 units per day.
- Prevent accidental fall. For example, keep your dwellings tidy, install supporting railing in the bathroom, be alert about slippery floors, avoid taking medicine that can cause drowsiness, or use a supporting cane if you have a problem balancing.
- Your doctor will determine whether or not you need medication for osteoporosis. There are 2 types of medication to treat osteoporosis. One type can be taken orally once a week with at least a glass of water when the stomach is empty, but you must delay taking any other medicine or food for an hour. The other type of medication consists of intravenous injection, which is once a year, and subcutaneous injections, which is every 6 months or daily or monthly. In any case, your doctor will discuss your condition as well as the advantages and disadvantages of each type of medication.
- Osteoporosis risks indicator and medication. To be considered are: whether there is any broken bone as a result of osteoporosis already, or the result of bone mineral density that indicates osteoporosis, or when existing osteopenia condition combined with a calculated FRAX score suggesting a 3% or more probability of a broken hip.
- Treatment follow-up. In general, after treatment, the bone density is checked every 1 or 2 years. In some cases, this will include blood test to determine how the bones are responding to treatment 3 – 6 months afterwards.











