Due to the advancements in an imaging technology, diagnosis of bile duct and pancreatic duct abnormalities by using endoscopic examination –ERCP (Endoscopic Retrograde Cholangiopancreatography) can be concurrently conducted with laparoscopic surgery to treat gallstones and bile duct stones. These combined procedures provide significant benefits, including reduced anesthetic-related risks, faster recovery time, shorter hospital stay, a quick return to daily life while helping to reduce medical expense.
Gallstone and bile duct stones
Gallstones are one of the most common diseases of the hepatobiliary system characterized as hardened deposits of digestive fluid that can form in the gallbladder. Gallstones are formed due to the precipitation of bile components, mainly calcium and cholesterol. Gallstones are highly prevalent and the majority are asymptomatic. Asymptomatic bile duct stones are usually detected in 6% to 12% of patients with gallstones. However, this incidence may rise to 20-25% in the elderly aged over 60.
Although gallstones are very common, if left untreated, it can potentially lead to serious complications and life-threatening conditions. Gallstones are more common in women, aged between 30-50. Gallstones may cause no signs or symptoms. Warning symptoms are bloating, abdominal discomfort or stomach upset, indigestion and sudden or rapidly intensifying pain in the upper right portion of the abdomen. If gallstones lodge in a duct and cause a blockage, the resulting signs may include jaundice present with yellowing skin and eyes which is more prevalently found in elderly patients.
Symptoms and severity
In an early stage of gallstones, patients might be asymptomatic. Common symptoms that patients seek for medical attention frequently include bloating, abdominal tightness or discomfort and intensifying pain in the upper right abdomen. If cholecystitis (an inflammation of gallbladder) develops, aggravating symptoms include severe and sudden pain in the upper right abdomen, high fever, nausea and vomiting.
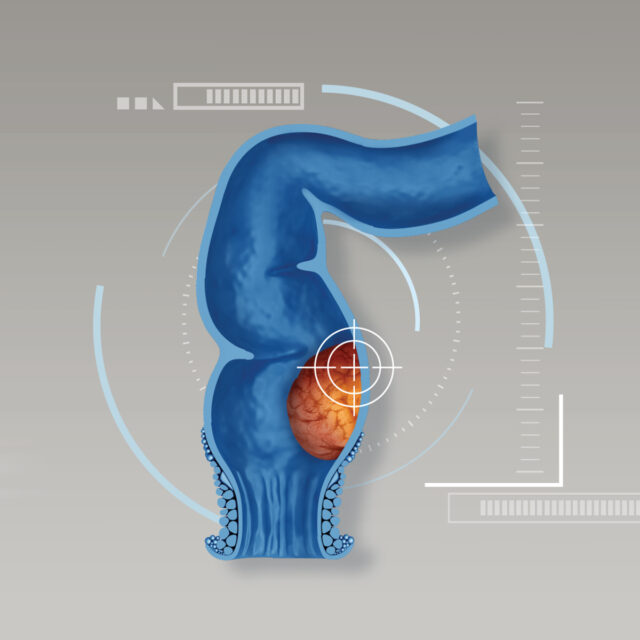
If gallstones become lodged in the bile ducts between the liver and the small intestine, it can cause inflammation of the bile duct which is called acute cholangitis. Acute cholangitis can block bile flow from the gallbladder and liver, causing pain, jaundice and fever. In some cases, bile duct stones are major contributing factor to acute pancreatitis –a sudden inflammation of the pancreas. Patient often show symptoms e.g. abdominal discomfort and severe pain in the right upper abdomen after eating 30 minutes to an hour. If abdominal pain severely progresses, patients mostly need to get medical treatment in the hospitals. Biliary colic defined as a dull pain in the middle to upper right area of the abdomen can happen when a gallstone blocks a bile duct, causing intense stomach pain. After receiving pain killer medicines, abdominal pain can be substantially alleviated if a gallstone that obstructs the bile duct and causes blockage is moved back and bile duct is unblocked. If this condition persists over time with repeated attacks, or if there are recurrent problems with gallbladder function, it can lead to chronic cholecystitis. However, if the blockage lasts longer than 24 hours without treatment, it might result in acute cholecystitis.
Acute cholecystitis is an emergency condition that is usually caused by a gallstone or biliary sludge that obstructs and causes the blockage of cystic duct, resulting in gallbladder inflammation and infection. If gallstones are passed to bile duct, it might cause bile duct infection (cholangitis) or acute pancreatitis. If left untreated, fatal complications such as sepsis can develop, causing an increased risk of death.
Diagnosis
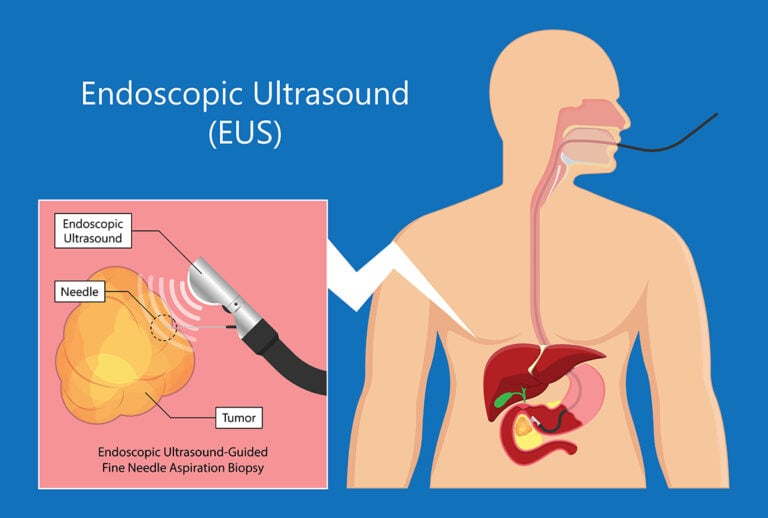
Advanced endoscopic examination, endoscopic ultrasound (EUS) can help identifying smaller stones that may be missed on an abdominal ultrasound. EUS is a minimally invasive procedure to assess gastrointestinal system. During EUS, doctor passes a thin, flexible tube (called endoscope) through the mouth and digestive tract. A small ultrasound device (transducer) in the tube produces sound waves that create detailed images of the lining and walls of the digestive tract, stomach and intestine. In addition, EUS can also detect some abnormalities that might be unseen by other endoscopic procedures e.g. liver mass, bile duct stones, gallstones and pancreatic mass.
During EUS, if abnomal mass is detected, EUS-guided real-time fine-needle aspiration biopsy can be performed to collect tissue sample for pathological assessment which the result can be obtained within 3-5 days.
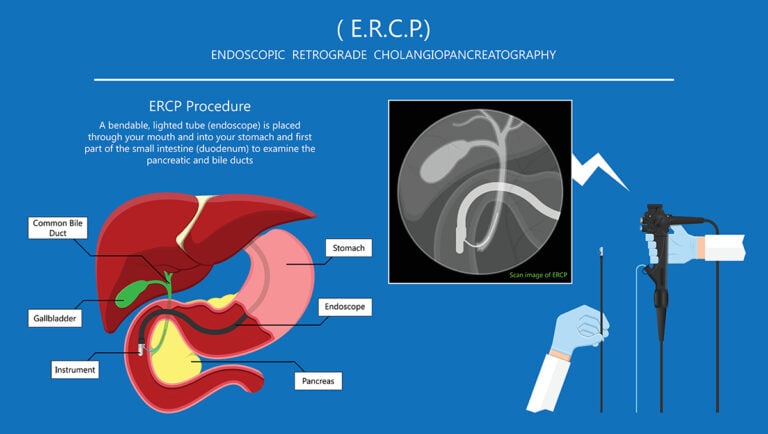
ERCP (Endoscopic Retrograde Cholangiopancreatography)
ERCP is an advanced endoscopic examination that has been used to treat pancreatic and billiary tract diseases. Main indications of ERCP include biliary obstruction (blockage of the bile duct system), jaundice, bile duct stones and bile duct tumors. ERCP uses a dye to highlight the bile ducts on X-ray images. A thin, flexible tube (endoscope) attached with a camera on the end is passed down the throat and into small intestine. The dye enters the ducts through a small hollow tube (catheter) passed through the endoscope. If bile duct blockage caused by gallstones is detected, a variety of balloons and baskets attached to the catheters can be passed into the ducts allowing stone removal. However, if abnormal mass which causes bile duct compression is detected, tissue samples can be removed for pathological assessment. The insertion of a tube into the bile duct (biliary drainage) can be commonly carried out to relieve jaundice when the bile ducts are blocked.
Nonetheless, ERCP is associated with a 3-5% risk of pancreatitis. Since the pancreatic duct locates closed to bile duct, thus ERCP might cause tissue irritation. However, mild post-ERCP pancreatitis can be resolved within 1-2 days after stop drinkng and eating. Main treatment involves intravenous fluid infusion and administration of pain killer medicines. Patients are highly recommended to stay over night at least 1 night in the hospital after the procedure for close monitoring of any complication that might arise.
Instructions before EUS and ERCP are similar to those with gastroscopy, including:
- No foods and drinks are allowed 6-8 hours before procedure.
- Certain drugs that affect blood coaggulation process e.g. antiplatelet and anticoagulant drugs must be discontinued 3-5 days before prodecure, depending on type of medication.
- Patients should keep the doctor informed if they have respiratory or heart disease. Physical assessment might be further required to evaluate patient’s condition before the procedure begins.
Treatment of gallstones and bile duct stones
To treat patients who have gallstones present with bile duct stones, or with other complicated conditions e.g. acute pancreatitis, obstructive jaundice or acute cholangitis, doctors might suggest ERCP and laparoscopic cholecystectomy in a combined procedure (one-step) in patients who are eligible.
Laparoscopic cholecystectomy is advanced MIS (minimally invasive surgery). During laparoscopic cholecystectomy, supported by advancements in HD vision system, 4K ultra-high definition camera substantially provides detailed images of gallbladder, bile ducts and surrounding organs in all dimensions. This advanced technology largely helps improving surgical performance, accuracy as well as safety, resulting in smaller incision, less pain and fewer postoperative complications such as reduced infection rates as well as faster recovery and a quick return to daily life.
In addition to a team of highly skilled surgeons who perform laparoscopic surgery and gastroenterologists, a multidisciplinary team of rehabilitation physicians, pharmacists and dietitians work closely to provide personalized postoperative care including nutrition advices, leading to faster recovery.
Treatment of gallstones and bile duct stones with ERCP and laparoscopic cholecystectomy at the same time helps to reduce procedure-related complications if these two procedures are conducted seperately (ERCP is firstly performed followed by laparoscopic cholecystectomy) such as billiary blockage or cholangitis while waiting for surgery after ERCP.
In addition, combined procedure enable the patients to undergo general anesthesia only once, resulting in lowered risk of anesthetic-associated effects. Minimally invasive surgery substantially shortens the hospital stay, leading to a faster recovery with an ability to walk within 4-6 hours after surgery. Moreover, pancreatitis and other postoperative complications significantly decrease if procedures are concurrently performed.
To reduce risks of gallstones, recommendations include: remain healthy with appropriate weight, avoid fatty or oily foods and eat more fish and high-fiber foods e.g. vegetable and fruits to reduce chance of bloating and indigestion. If gallstones develop, to achieve the best possible outcomes, treatment should be conducted by expert and highly experienced multidisciplinary team in the hospitals with international standard. If abnormal sign or symptom arise, it should not be overlooked, immediate medical attention must be sought to receive timely and effective treatment with minimized risks of serious complications that might happen in the future.