What Is Skin Cancer?
Skin cancer begins when abnormal cells form a growth on the skin. These malignant cells can invade and destroy healthy tissue—and may even break away and spread (metastasize) to other parts of the body
There are several types of skin cancer, with basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) being the most common. These non-melanoma skin cancers are typically slow-growing and highly treatable when caught early. The most aggressive type is melanoma, which is less common but far more likely to spread, making it more challenging to treat.
Most skin cancers develop on sun-exposed areas, as ultraviolet (UV) radiation from sunlight and tanning beds is the leading cause. You can significantly lower your risk by protecting your skin—wear protective clothing, seek shade, and use broad-spectrum sunscreen (SPF 30+)
However, some skin cancers appear on areas not typically exposed to the sun, indicating other risk factors (e.g., genetic predisposition or chemical exposure) may be involved. To detect these early, perform regular skin self-checks for any new or changing spots—and consult your healthcare provider if you notice anything concerning
Sources:
- https://www.mayoclinic.org/diseases-conditions/skin-cancer/symptoms-causes/syc-20377605
- https://healthencyclopedia.org/skin-cancer/?utm_source=chatgpt.com#types
- https://www.thesun.ie/health/15219836/ireland-heatwavev-health-alert-uv-warning
- https://www.bangkokhospital.com/en/phuket/content/most-common-skin-cancer-basal-cell-carcinoma-what-is-it-treatment-and-how-to-prevent-bpk
Skin cancer signs and symptoms
Skin cancers don’t all look alike—they can mimic benign conditions like warts or flaky patches, which makes early detection vital. It’s important to examine your skin regularly and consult a healthcare provider if you notice any of the following:
- New, growing, or changing spots: Any new bump, mole, or spot—or one that’s enlarging or evolving—should be checked.
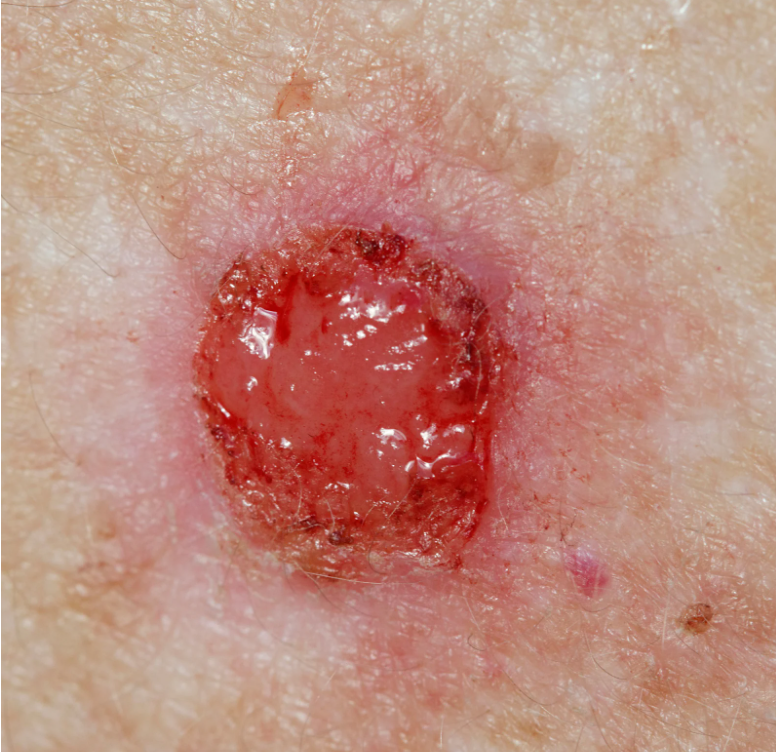
- Non-healing sores: A sore that bleeds, crusts, or persists without healing for several weeks is a red flag.
- Rough, scaly patches: Especially red, crusty areas that may bleed or itch—common in squamous cell carcinoma.
- Wart-like growths: Rough, raised bumps resembling common warts could be a sign of skin cancer.
- Pearly or shiny bumps: Smooth, translucent or waxy bumps—often with visible blood vessels—are typical of basal cell carcinoma.
- Changing moles: Look for moles that are new or changing in size, shape, color, or texture—especially those with odd shapes, uneven borders, or multiple colors.
Sources:
- https://www.cancer.org/cancer/types/basal-and-squamous-cell-skin-cancer/detection-diagnosis-staging/signs-and-symptoms.html
- https://www.mdanderson.org/cancer-types/skin-cancer/skin-cancer-symptoms.html
Signs and symptoms of basal cell skin cancer
Basal Cell Carcinoma (BCC): Common Signs & Symptoms
Basal cell carcinomas typically develop on sun-exposed skin—like the face, neck, scalp, and arms—but can appear anywhere on the body
In individuals with lighter skin tones, BCC may present as:
- Small, shiny bumps that are pink or red, translucent, and pearly; they sometimes include flecks of blue, brown, or black.

- Pink growths with raised, rolled edges and a central depression that may feature tiny blood vessels radiating outward like spokes
- Flat, firm, pale or yellowish patches that resemble scars
- Raised, reddish areas that may itch

- Non-healing sores—often oozing or crusted—that persist or recur
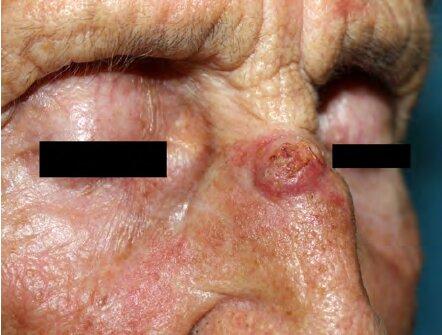
In people with darker skin, BCC is less common but can appear similarly—translucent, shiny, or raised—though often darker in color

Sources:
- https://www.cancer.org/cancer/types/basal-and-squamous-cell-skin-cancer/detection-diagnosis-staging/signs-and-symptoms.html
- https://www.bangkokhospital.com/en/phuket/content/most-common-skin-cancer-basal-cell-carcinoma-what-is-it-treatment-and-how-to-prevent-bpk
- https://www.researchgate.net/publication/221921390_Basal_Cell_Carcinoma
Signs and symptoms of squamous cell skin cancer
Squamous cell carcinoma (SCC) is a type of skin cancer that can develop in various areas of the body, with its appearance and location often influenced by skin tone and sun exposure.
Common Locations Based on Skin Tone
- Lighter Skin Tones: SCCs frequently appear on sun-exposed areas such as the face, ears, neck, lips, and the backs of the hands.
- Darker Skin Tones: In individuals with darker skin, SCCs are less common but may develop in areas that are less exposed to the sun, including the palms, soles, genital region, and under the nails.
Appearance of SCC
SCCs can manifest in various forms, including:
- Rough, scaly red or darker patches that may crust or bleed.

- Raised growths or lumps, sometimes with a central depression.

- Open sores that may ooze or crust and do not heal or heal and then return.

- Wart-like growths.

These lesions can vary in color, ranging from red or pink to purple, gray, brown, or black, depending on the individual’s skin tone.
Less Common Locations
SCCs can also develop in less typical areas, such as:
- Genital regions.
- Scars or skin sores elsewhere on the body.
These occurrences are less frequent but still significant.
When to Consult a Healthcare Provider
It’s advisable to seek medical attention if you notice:
- A sore or growth that doesn’t heal within a couple of months.
- A new growth or a change in an existing mole or spot.
- A lesion that bleeds, crusts, or reappears after healing.
Early detection and treatment are crucial for effective management of SCC.
Sources:
- https://www.skincancer.org/skin-cancer-information/squamous-cell-carcinoma/scc-treatment-options/
- https://www.aad.org/public/diseases/skin-cancer/types/common/scc
- https://www.bangkokhospital.com/en/phuket/content/skin-cancerunderstanding-cutaneous-squamous-cell-carcinoma-cscc-bpk
- https://www.mayoclinic.org/diseases-conditions/squamous-cell-carcinoma/symptoms-causes/syc-20352480
- https://www.cancer.org/cancer/types/basal-and-squamous-cell-skin-cancer/detection-diagnosis-staging/signs-and-symptoms.html
Other ways basal and squamous cell carcinomas can look
Both basal and squamous cell skin cancers can also develop as a flat area showing only slight changes from normal skin.
These and other types of skin cancers can also look different from the descriptions above. This is why it’s important to have a doctor check any new or changing skin growths, sores that don’t heal, or other areas that concern you.
Sources:
- https://www.cancer.org/cancer/types/basal-and-squamous-cell-skin-cancer/detection-diagnosis-staging/signs-and-symptoms.html
- https://www.bangkokhospital.com/en/phuket/content/skin-cancerunderstanding-cutaneous-squamous-cell-carcinoma-cscc-bpk
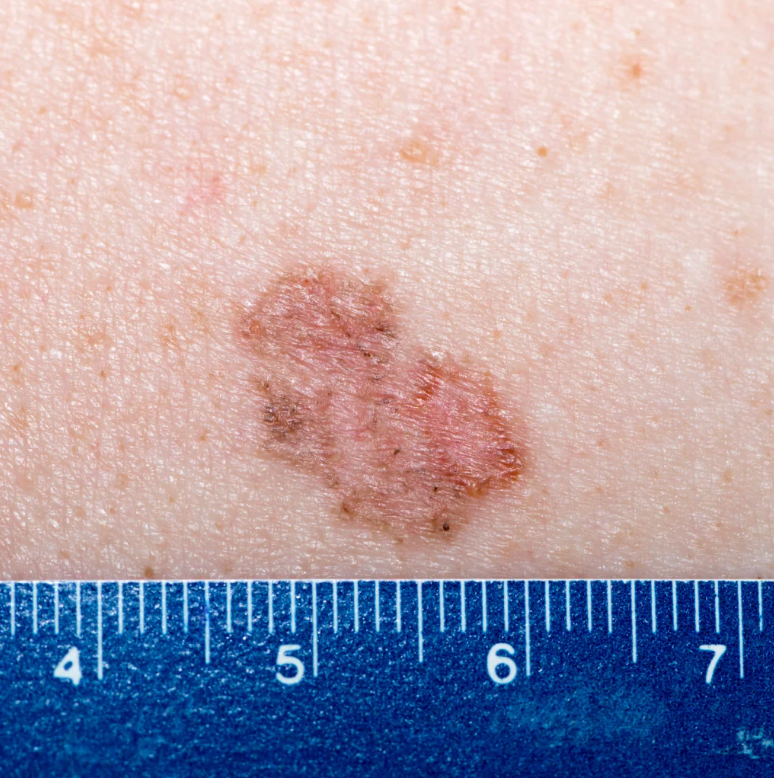
Signs and symptoms of melanoma
Melanoma is the most dangerous type of skin cancer. It can look harmless at first—like a small mole or spot—but if not caught early, it can spread quickly. That’s why it’s important to know what to look out for.Traditionally, doctors used the ABCD rule to check moles. But now, they also include EFG to help spot early, fast-growing types like nodular (pink) melanoma, which may not follow the usual ABCD signs.
The ABCD + EFG Rules: 7 Key Signs to Watch For
- A – Asymmetry
One side of the spot or mole looks different from the other. - B – Border
Edges are uneven, jagged, or blurred—not smooth or round. - C – Color
The mole has more than one color—like black, brown, red, white, blue, or gray. - D – Diameter
Larger than 6 mm (about the size of a pencil eraser), but can be smaller when caught early. - E – Evolution
It’s changing—getting bigger, darker, or different in shape. - F – Firm
Feels hard or solid when you press it. - G – Growing
Getting bigger over time, especially over a month or more.
Extra Clues: The 7-Point Checklist
Recommended by UK skin cancer experts to improve early detection.
Major Warning Signs (Big Red Flags)
- A new spot that’s growing
- A mole that’s changing shape (especially uneven edges)
- A mole changing color (uneven or new shades)
Minor Warning Signs
- Larger than 7 mm
- Redness or swelling (inflammation)
- Crusting, scabbing, or bleeding
- Itching or unusual sensations
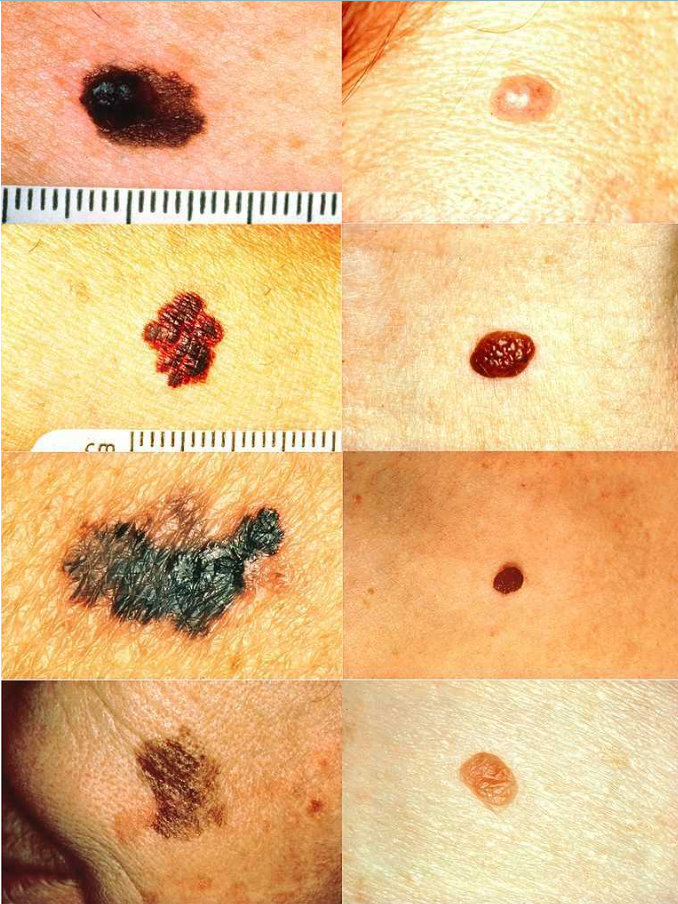
Melanoma Detection. On the left side from top to bottom: melanomas showing (A) asymmetry, (B) a border that is uneven, ragged, or notched, (C) coloring of different shades of brown, black, or tan and, (D) diameter that had changed in size. The normal moles on the right side do not have abnormal characteristics (no asymmetry, even border, even color, no change in diameter). National Cancer Institute Skin Cancer Foundation
From: Melanoma of the Head and Neck
Source: https://www.ncbi.nlm.nih.gov/books/NBK513248/figure/article-25328.image.f3/
When to See a Doctor:
- If you have one major sign plus one minor, or
- If you have three minor signs,
it’s time to get your skin checked by a dermatologist.
Your Skin Can Save Your Life
Melanoma is highly treatable if caught early. Look for any new, changing, unusual, or growing spots on your skin—even ones that don’t look dark or scary.
If in doubt, check it out.
Source:
- https://www.uptodate.com/contents/melanoma-clinical-features-and-diagnosis?search=MELANOMA&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H2682382315%3E
- https://bjgp.org/content/63/610/e345
- https://www.bangkokhospital.com/en/phuket/content/skin-cancer-updated-7-alarming-signs-for-melanoma-bpk
Diagnosis
- Clinical exam & history
- Your doctor (often a dermatologist) will assess the lesion’s appearance and ask about changes, symptoms, sun exposure, medical/family history
- A dermatoscope—a special magnifying lighted tool—may be used to examine lesions more closely.
- Skin biopsy
- The definitive way to diagnose is via biopsy—removing all or part of the suspicious skin and examining it under a microscope
- Types include shave, punch, or excisional biopsy.
- Further evaluation & staging
- If biopsy confirms cancer, additional tests (like lymph node biopsy, imaging, or blood tests) may be needed, especially if there’s concern the cancer has spread.
Treatment Options
Treatment depends on the type of skin cancer—BCC, SCC, melanoma—or other rare types:
A. Non-melanoma skin cancers (BCC & SCC)
- Surgery
- Standard excision: Commonly removing the tumor plus a margin of healthy tissue
- Mohs micrographic surgery: Layer-by-layer removal with immediate microscopic examination—highest cure rates (≈97–99%) and tissue-sparing.
- Curettage and electrodesiccation (C&E)
- Scraping and cautery, usually for small, low-risk lesions. Quick but less margin-controlled.
- Cryotherapy
- Freezing the tumor, mainly for precancerous or superficial lesions.
- Topical therapies
- Creams like 5-fluorouracil or imiquimod for superficial BCC or actinic keratosis
- Photodynamic therapy
- Combination of a photosensitizing agent and light to destroy cancerous tissue.
- Radiation Therapy
- Used when surgery isn’t ideal, or on certain locations/patient health conditions.
- Systemic therapies
- For advanced cases: chemotherapy, targeted agents (e.g., EGFR inhibitors), or immunotherapy.
B. Melanoma
- Wide surgical excision with margins depending on depth/stage
- Sentinel lymph node biopsy for intermediate/thicker melanomas to assess spread.
- Adjuvant treatments include:
- Immunotherapy (e.g., checkpoint inhibitors) and targeted therapies (e.g., BRAF + MEK inhibitors) for BRAF-mutated or advanced melanomas.
- Clinical trials and investigational treatments (e.g., cellular therapies) are increasingly available.
C. Rare skin cancers (e.g., Merkel cell carcinoma)
- Generally treated with surgery plus radiation, and immunotherapy if advanced.
Choosing the Right Treatment
- Early-stage non-melanoma: surgery (often Mohs) or local therapies (like C&E, cryotherapy, topical agents, photodynamic therapy).
- When surgery isn’t feasible: radiation, topical, or systemic options.
- Advanced or high-risk disease: may require combination of surgery, radiation, systemic therapy.
- Melanoma: surgical excision is cornerstone; advanced cases often get lymph node biopsy, immunotherapy, or targeted treatment.
Aftercare & Follow-Up
- Regular skin exams to detect recurrence or new lesions.
- Monitor surgical sites.
- For melanoma, follow-up includes imaging and lab tests as guided by stage.
Summary Table:
| Skin Cancer Type | Diagnosis | First-line Treatment | Advanced/High-risk Treatment |
|---|---|---|---|
| BCC / SCC (non-melanoma) | Dermoscopy + biopsy | Mohs or excision | Radiation, topical, photodynamic, systemic |
| Melanoma | Biopsy + staging | Wide excision ± lymph node biopsy | Immunotherapy, targeted therapy (e.g., BRAF), trials |
| Merkel cell & others | Biopsy ± lymph node biopsy | Surgery + radiation | Immunotherapy |
Sources:
- https://www.cancer.org/cancer/types/basal-and-squamous-cell-skin-cancer/detection-diagnosis-staging/how-diagnosed.html
- https://www.aad.org/public/diseases/skin-cancer/types/common/melanoma/diagnose-treat
- https://www.cancer.org/cancer/types/basal-and-squamous-cell-skin-cancer/detection-diagnosis-staging/how-diagnosed.html
- https://www.aafp.org/pubs/afp/issues/2020/0915/p339.html
- https://www.mayoclinic.org/diseases-conditions/skin-cancer/diagnosis-treatment/drc-20377608
High-Risk Skin Cancer Treatment Options:
Mohs Surgery vs. Wide Excision: What’s the Difference?
Both procedures are used to remove skin cancer, but they are done differently and used for different reasons.
Mohs Surgery (Also called Mohs Micrographic Surgery)
What it is:
A very precise surgery where the cancer is removed layer by layer, and each layer is checked under a microscope right away until no cancer is left.
Best for:
- Skin cancers on the face, ears, nose, eyelids, fingers, or other delicate areas
- When it’s important to save as much healthy skin as possible
- Cancers that have come back after treatment
- Tumors with unclear edges
- High risk subtype of skin cancer such as micronodular or infiltrating basal cell carcinoma and moderate to poor differentiate squamous cell carcinoma
Pros:
- Highest cure rate (up to 99%) for certain skin cancers
- Removes the least amount of healthy tissue
- Done in one visit, usually under local anesthesia
- Minimal scarring when done properly
Wide Local Excision (WLE)
What it is:
The doctor removes the cancer along with a wider area of normal-looking skin around it, just to be sure all the cancer is gone. The tissue is then sent to a lab, and results come back a few days later.
Best for:
- Melanoma
- For low risk subtype of skin cancer such as nodular or superficial basal cell carcinoma and well differentiate squamous cell carcinoma
- Cancers located on parts of the body where removing extra skin is not a big concern (like arms, back, legs)
Pros:
- Often used for melanoma, which may need a wider margin
- Can be done under local or general anesthesia depending on size
Key Differences at a Glance
| Feature | Mohs Surgery | Wide Excision (WLE) |
|---|---|---|
| How cancer is removed | Layer by layer, examined during surgery | Entire lump + surrounding skin removed at once |
| Precision of margin examination | 100% margin peripheral and deep en face margin examination | 1-2%margin of vertical section evaluated |
| Where tested | On-site lab during surgery | Sent to external lab (results in days) |
| Tissue removed | Smallest possible amount layer by layer | Wider area removed to ensure margins |
| Best for | Face, ears, nose, and high-risk areasHand, feet, and genital area | Melanoma, less critical area tissue preservation BCC or SCC |
| Cure rate | Very high (especially for BCC/SCC) | Also high, especially for melanoma |
| Scar size | Usually smaller | May be larger depending on tumor size |
| Cost | Generally more expensive | Generally less expensive |
Which One Do I Need?
That depends on:
- The type of skin cancer (e.g., BCC, SCC, melanoma)
- Where it is located
- How big and deep the tumor is
- Whether it has come back before
Your dermatologist or surgeon will recommend the best option based on your case.
Source:
National Comprehensive Cancer Network Clinical Practice Guideline in Oncology 2025 (NCCN guideline)
Low-Risk Skin Cancer Treatment Options
| Treatment Option | Pros (Advantages) | Cons (Disadvantages) | Chance Cancer Comes Back in 5 Years |
|---|---|---|---|
| Standard Wide Excision | – Tissue margins checked in the lab (more accurate)- Good long-term results | – May need another surgery if cancer isn’t fully removed | BCC: 0.8–17.4%SCC: 5–8% |
| Shave Removal | – Quick and low cost- No stitches needed | – May not remove all the cancer- Margins not checked under microscope | BCC: 0.5–30%SCC: Not recommended |
| Electrodesiccation & Curettage | – Quick and low cost- No stitches needed | – No lab check of cancer edges- May leave a scar or dip | BCC: 1.2–40%SCC in situ: 3–8% |
| Cryotherapy (Freezing) | – Quick and low cost- No stitches needed | – No lab check- May need more than one treatment- Can cause blisters | BCC: 5–39%SCC: Not well reported |
| Topical Creams (Imiquimod or 5-FU) | – Lowest cost- Non-surgical- Approved for surface-level BCC | – Must be used daily for at least 6 weeks- Can cause skin irritation | BCC: ~11% (Gollnick et al, 2008)SCC: Not well reported |
| Other Treatments (e.g., Photodynamic Therapy, Radiation) | – Useful in some cases if available | Not specified |
Note:
- BCC = Basal Cell Carcinoma
- SCC = Squamous Cell Carcinoma
- SCC in situ (SCIS) = Early-stage SCC
- Margin assessment = Checking edges of removed tissue under a microscope to confirm cancer is gone
Source: