“The Only ICU in the Region Offering Private Isolation Rooms”



At Bangkok Hospital Phitsanulok (BPL), our ICU sets itself apart through its commitment to patient-centered care — most notably by offering individually separated ICU rooms, a rarity in the region. This distinction is more than just structural; it directly enhances clinical outcomes, safety, and patient experience.
Why do private ICU rooms matter?
Private ICU rooms bring a host of critical advantages that elevate the standard of care:
-
Infection Control:
Private rooms significantly reduce the risk of cross-infection between critically ill patients. By limiting contact and shared airspace, we enhance infection prevention protocols and safeguard both patients and medical personnel. -
Personalized Care:
Individual rooms allow healthcare providers to tailor treatments more precisely, based on the severity and urgency of each patient’s condition — improving responsiveness and outcomes. -
Privacy and Dignity:
Private settings support patients’ emotional and psychological needs, especially for those dealing with stress, depression, or other sensitive health conditions. A dedicated space fosters dignity, calm, and reassurance during critical moments. -
Environmental Control:
Private ICU rooms allow for better control over temperature, humidity, and noise levels — all of which play a vital role in patient recovery and comfort. -
Optimized Equipment Management:
A separate environment simplifies the organization and deployment of medical equipment, reducing clutter and streamlining workflows for more efficient, safer care. -
Enhanced Monitoring:
Private rooms provide an optimal setting for continuous and focused monitoring, enabling clinicians to detect changes quickly and intervene promptly when needed.In sum, the inclusion of private rooms in our ICU is not merely a facility upgrade — it’s a strategic investment in safer, more effective, and compassionate critical care. At BPL, we believe that in moments of medical crisis, patients deserve not only the best treatment but also the best environment in which to heal.
12 Truths You Should Know Before Entering the ICU
What to Expect—And What to Prepare For
Truth #1: The Nature of the ICU
Patients admitted to the Intensive Care Unit (ICU) are often in critical condition. Their health status can change dramatically—either for better or worse—within moments. In this sense, the ICU is characterized by uncertainty. But amidst this uncertainty, one thing is certain: the presence of a highly specialized, multidisciplinary critical care team, equipped with cutting-edge technology and knowledge. The ICU is the hospital’s most advanced unit, where everyone is committed to walking beside the patient through this life-threatening journey—until they emerge stronger, like the clear skies after a storm.
Truth #2: The Pinnacle of Care
Each ICU patient receives care at the highest possible standard, aimed at maximizing survival. The “six pinnacles of critical care” include:
-
Excellence in Treatment: With the best professionals, top-tier equipment, well-structured systems, and up-to-date medical knowledge, the ICU is akin to a five-star VIP suite—except its goal is saving lives.
-
Excellence in Physicians: Intensivists and critical care doctors are specifically trained to manage life-threatening conditions with precision.
-
Excellence in Teamwork: A multidisciplinary team—from nurses and pharmacists to respiratory therapists and nutritionists—works in harmony to provide comprehensive care.
-
Excellence in Equipment: ICU devices enable real-time monitoring, advanced diagnostics, and life support. These tools are continuously evolving with the latest in medical technology.
-
Excellence in Medication: ICU medications are potent, often with complex mechanisms tailored for severe conditions.
-
Excellence in Cost: High-quality care comes with high costs—driven by expert personnel, state-of-the-art machines, and advanced pharmaceuticals.
Truth #3: A Multidisciplinary Approach
ICU care involves experts from various fields, including attending specialists, ICU nurses, pharmacists, nutritionists, and physical therapists. Though care is collaborative, one lead physician always takes primary responsibility for the patient’s overall condition and treatment plan.
Truth #4: United in Support of the Lungs
When a patient can no longer breathe independently—known as respiratory failure—oxygen support is vital. Depending on the severity, this can range from simple oxygen masks or nasal cannulas to mechanical ventilation via intubation. In prolonged cases, a tracheostomy may be needed to ensure long-term, safe respiratory support.
Truth #5: Surviving Shock
Shock occurs when blood flow—and therefore oxygen and nutrients—fails to reach vital organs, risking organ failure and death. Emergency treatment includes:
-
Stabilizing circulation: By administering IV fluids or blood transfusions while monitoring central venous pressure to avoid complications such as pulmonary edema.
-
Treating the cause: Whether it’s bleeding, infection, or a heart attack, addressing the root cause is critical—even if surgical intervention is required.
-
Supporting failing organs: Ventilation may be needed for respiratory failure; dialysis may be required for kidney failure. Each decision is discussed thoroughly with the patient’s family to ensure appropriateness.
Truth #6: Nutrition is Non-Negotiable
Nutrition is a critical part of ICU care. If no medical contraindications exist, enteral feeding (via the digestive tract) is preferred and should begin as early as possible. If this route is inadequate or impossible, parenteral nutrition (via IV) is provided. This support significantly boosts recovery, helping patients regain strength and functionality faster.
Truth #7: CPR and the Continuation of Life
Cardiopulmonary resuscitation (CPR) can revive a patient whose heart or breathing has stopped. While success rates remain at 5–10%, proper and timely CPR can make a difference. However, it may not be appropriate in cases where brain and muscle function has irreversibly ceased, as indicated by:
-
No pupillary response to light at 24 hours
-
No corneal reflex at 24 hours
-
No limb withdrawal to painful stimuli at 24 hours
-
No muscle activity at 24 or 72 hours
Truth #8: Uncertainty is the Only Certainty
Unlike other wards, the ICU presents rapid changes that can be unpredictable. Despite round-the-clock surveillance, advanced medical tools, and continuous care, outcomes remain uncertain. Sometimes, despite every effort, the critical illness may prevail. Acceptance of this reality is key.
Truth #9: Preparation is Everything
Both patients and families must prepare—emotionally and logistically—for an ICU stay. Designate 1–2 family members to be involved in medical decisions. Discuss treatment preferences, and remain engaged with the healthcare team. Family participation supports better planning, care alignment, and dignity in decision-making.
Truth #10: Embrace Acceptance
While the aim is always recovery, outcomes are not always favorable. If a patient’s condition worsens despite maximal care, a shift toward palliative care may be appropriate—to prioritize comfort and quality of life. Accepting this truth allows a more peaceful and humane end-of-life experience, guided by compassion and understanding.
Truth #11: Crisis Doesn’t End at Discharge
Surviving the ICU doesn’t mean the battle is over. Patients often face lingering issues—muscle weakness, depression, PTSD. Continued rehabilitation and emotional support are crucial. Families must understand and participate in the post-ICU journey to help patients reintegrate into life and society.
Truth #12: The Cost of Survival
ICU care is resource-intensive—driven by high-end medications, specialized equipment, and expertly trained professionals. These elements make ICU treatment costly, whether in public or private hospitals. However, cost never overrides care. No patient is denied treatment because of financial limitations.
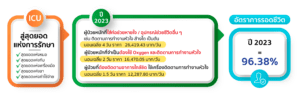
Separate ICU patients, serious/light, how many days to stay, how much does it cost in 2023?
| • Patients requiring invasive mechanical ventilation or life-support interventions such as continuous cardiac monitoring, dialysis, or other advanced therapies. |
Average Length of Stay: 4 days Average Cost per Day: THB 26,419.43 |
| • Patients requiring continuous oxygen therapy and close cardiac monitoring, without the need for intubation or full life support systems. |
Average Length of Stay: 2 days Average Cost per Day: THB 16,470.05น |
| • Patients who are stable but still need close monitoring, typically via cardiac monitoring systems, to track any potential deterioration. |
Average Length of Stay: 1.5 days Average Cost per Day: THB 12,287.80 |
Survival Rate in ICU (2023)= 96.38%