Esophagogastroduodenoscopy, EGD
1. Basic Information
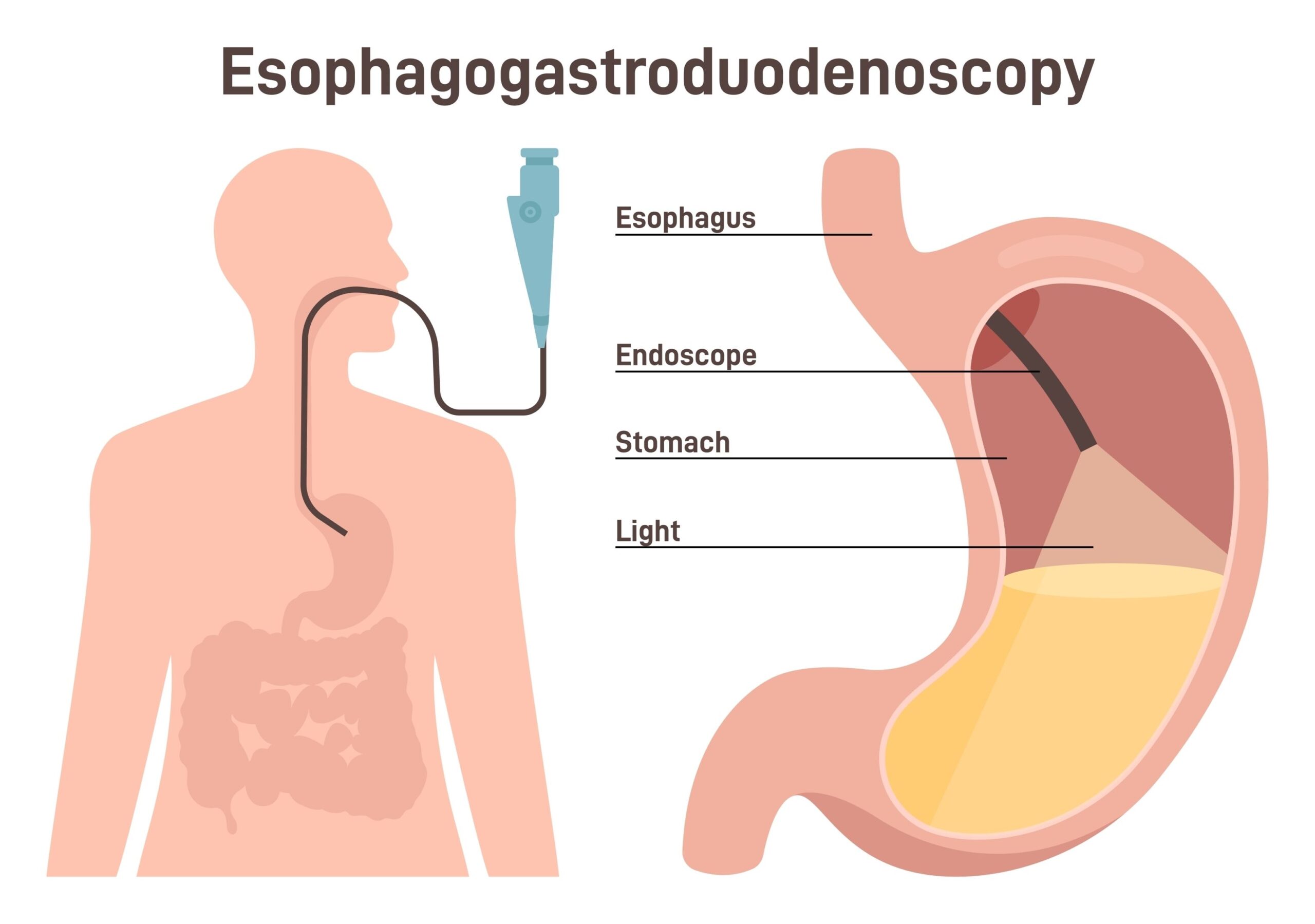
An upper gastrointestinal endoscopy is a procedure to examine the lining of the esophagus, stomach, and the upper part of the small intestine by inserting a small flexible tube with a tiny camera and light at the end, through the mouth. This allows visualization of the larynx, esophagus, stomach, and the upper part of the small intestine. The doctor can view through a monitor or camera to diagnose the cause of symptoms and may take tissue samples from abnormal areas for diagnostic confirmation and more accurate treatment.
2. Risks and Side Effects of Examination and Treatment
2.1. General Risks
• Sore throat caused by the friction of the endoscope
• Throat numbness due to local anesthetic
• Bloating is a common occurrence because the doctor has to blow air into the stomach during the endoscopy. However, this condition is temporary and improves once the body expels the air.
2.2. Specific Risks
• Perforation of the stomach and esophagus is a rare risk (1:1,000). If this risk occurs, the patient must be hospitalized for treatment via endoscopy or surgery to repair.
• Bleeding in the stomach due to tissue sampling, which usually results in small wounds that stop bleeding on their own. However, if the patient is taking blood-thinning medications, it can increase the risk of internal bleeding. In case of bleeding, the doctor will treat it by stopping the bleeding via endoscopy, interventional radiology, or surgery.
• Aspiration of food into the lungs due to insufficient fasting has a chance of less than 1:10,000.
• Dizziness from sedative or pain medication effects, such as allergic reactions, is a rare condition that occurs in about 1:10,000. It can be monitored and corrected with medication to counteract the effects.
• Broken or dislodged teeth. Patients with loose teeth or removable dentures should remove them before the endoscopy.
3. Pre- and Post-Procedure Instructions
3.1. Pre-procedure Instructions for Patients
3.1.1. Abstain from water and all types of food from midnight or at least 6 – 8 hours before the examination to prevent respiratory obstruction caused by vomiting and aspiration during the procedure. If it is necessary to take medication, consult the examining doctor or inform the staff in the endoscopy room.
3.1.2. Maintain oral and dental hygiene (the night before and the morning of the examination) to prevent oral and upper respiratory tract infections. Removable dentures should be taken out before the endoscopy to avoid dislodgement and airway obstruction.
3.1.3. Inform the doctor of any underlying diseases or medication allergies you have, such as allergies to local anesthetics, painkillers, or sedatives. If the patient is taking platelet aggregation inhibitors such as aspirin, clopidogrel (Plavix), pletal, or anticoagulants like warfarin, inform the doctor and stop taking these medications for at least 7 days before the examination to prevent bleeding. If in doubt about the regular medications affecting the examination, consult the examining doctor.
3.1.4. Do not bring valuables to the hospital on the day of the endoscopy. Those with dentures or contact lenses should remove them before entering the examination room.
3.1.5. Arrive at the hospital at least 1 hour before the examination time (with a relative). If traveling by private car, a relative who can drive should accompany you because the effects of sedatives or pain relief medication can impair driving ability for 24 hours.
3.2. Post-procedure Instructions for Patients
3.2.1. Let the patient rest in bed to observe symptoms for about 30 – 60 minutes or until fully awake.
3.2.2. Observe for any abnormal symptoms such as severe abdominal pain, vomiting or blood in stools, difficulty breathing or shallow breathing, low blood pressure, dizziness, fainting, deep sleep, or difficulty awakening. Report to the doctor immediately if these occur.
3.2.3. Throat numbness will subside within 1 hour. During this time, refrain from eating or drinking until the numbness disappears.
3.2.4. When the throat numbness subsides, try eating bread. If there is no choking, consume soft foods. Some patients may experience slight soreness in the throat due to the endoscope, which will go away shortly.
3.2.5. Patients should see the doctor on their scheduled appointment (especially for those with tissue samples sent for examination to receive the results). See the doctor before the appointment if there are complications or to receive medication.
3.2.6. When the doctor allows a patient to be discharged, a caretaker should assist during the journey home. Do not drive or operate machinery or climb to high places within 24 hours, especially for those who received sedatives or painkillers during the endoscopy. After returning home, a nurse will call to check on the patient’s condition post-endoscopy.
4. Other Alternatives
4.1. Diagnostic testing by swallowing barium (Barium Swallow)
4.2. Diagnostic testing via UGI Barium study