Painful bowel movement with some bleeding can bring tears to the point that some may not want to go to the bathroom. Some may find a palpable polyp that causes even more distress. Medication may not improve the situation. These are tell-tale signs that you may have the popular condition among patients with constipation, although “anal fissure” is not a household name.
What is Anal Fissure?
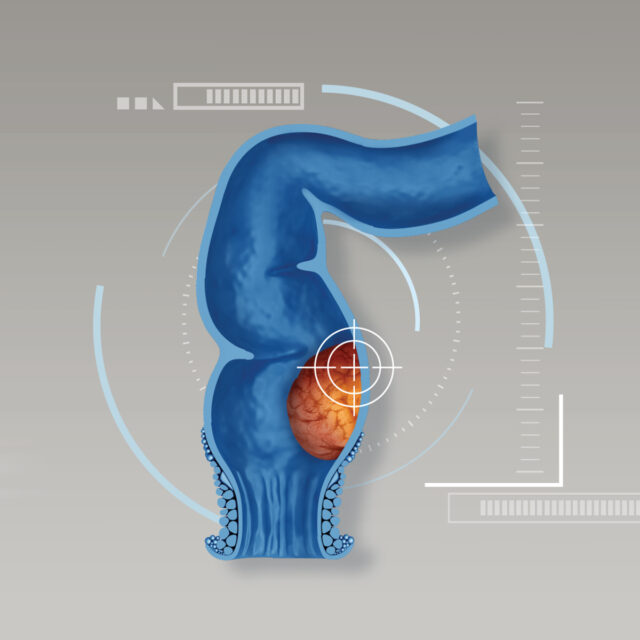
An anal fissure is a small tear in the tissue that lines the anus which may go deep in the muscle of anal sphincter. It is a common condition and is similar to hemorrhoids which can be easily mistaken and ignored.
Symptoms
- Pain during bowel movements with hard stool. Its burning pain can be compared to a small wound and can persist for hours after bowel movements in cases of bigger tear.
- Bright red, fresh blood on the stool or toilet paper after a bowel movement.
- A palpable polyp or lump around the anus area.
- Itchiness around the anus with unusual smell.
- If it is very painful, it may be difficult to urinate or incontinence.
Cause of Anal Fissure
Most of anal fissure is caused by heavy straining to defecate from diarrhea or constipation. In some case, the tear is deep into the inner anal sphincter muscle and create inflammation and contraction, resulting in less blood supply to the wound which makes it harder to heal. It will eventually turn into a chronic wound. The inflammation in patients with chronic anal fissure will become a sentinel pile around the wound. However, the similar sentinel pile can be found in mom after given birth, patients with cancer, tuberculosis, syphilis, and intestine inflammation.
Diagnosis
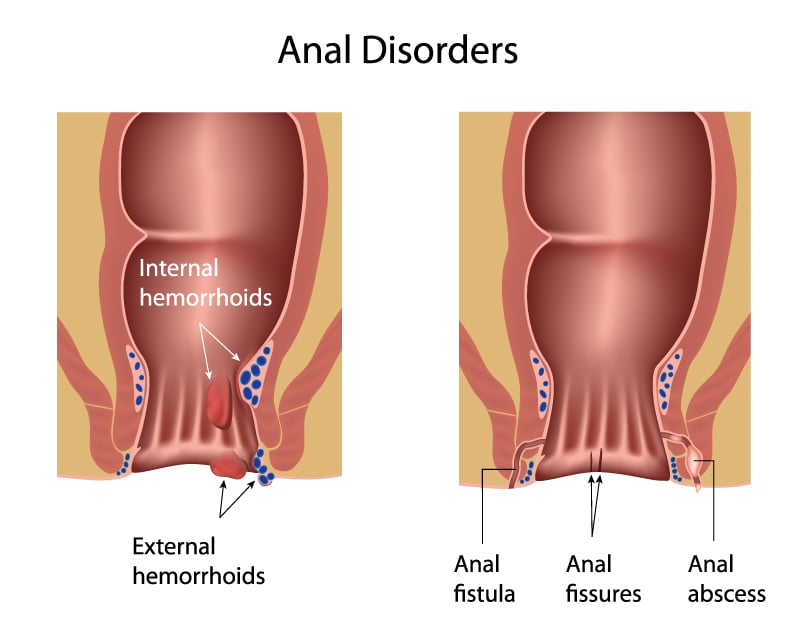
Doctor can diagnose anal fissure by taking a detailed patient’s history and physical examination to rule out other conditions such as hemorrhoids, anal fistula, etc. A thorough physical examination can detect the fissure either in the front or the back of the anus. Differential diagnosis may be necessary such as endoscopy for tissue biopsies, and other laboratory tests for comorbidities such as syphilis and HIV.
Treatment for Anal Fissure
Anal fissure is a common condition which should not be neglected. If left untreated, it may cause a complication of anal fistula or concerns about a lump which may become malignant. So, if you suspect that you have an anal fissure, you should consult a specialist to diagnose and treat correctly. The treatments can be divided into surgical and non-surgical treatments.
- Non-surgical Treatment is suitable for patients with an early stage of anal fissure:
- Drink 6-8 glasses of water
- Consume more fruits and vegetables
- Take laxatives to relief constipation, make stool softer, and reduce inflammation and pain
- Soak in warm water for 15 minutes 2-3 times a day to reduce pain and increase blood flow.
- Use topical medication to relax the sphincter and increase blood flow.
- Inject Botulinum Toxin to relax sphincter muscle and increase blood flow.
- Surgical Treatment is suitable for patients who suffered from anal fissure for more than 6 – 8 weeks and medication does not make it better or symptoms persisted when stop medication. A lateral internal sphincterotomy is a minimally invasive surgery about 1 cm in size to correct the internal sphincter that is inflamed and contracted while saving the external sphincter. The benefits of this treatment include:
- Local or spinal anesthesia without the need for systemic anesthesia
- Short hospital stay and quicker recovery
- 95% chance of a cure
- Hemorrhoid can be corrected at the same time
Anal fissure is common but the pain is high. Prevent constipation and take time to pass bowel movement. If symptoms persist, please consult a specialist to diagnose and treat anal fissure during the early stages. Patients who have chronic anal fissure should get suitable treatment. For patients who require surgery, minimally invasive surgery can result in less pain, quicker recovery and increased chance of a cure. Lastly, patients no longer need to withstand pain during a bowel movement.